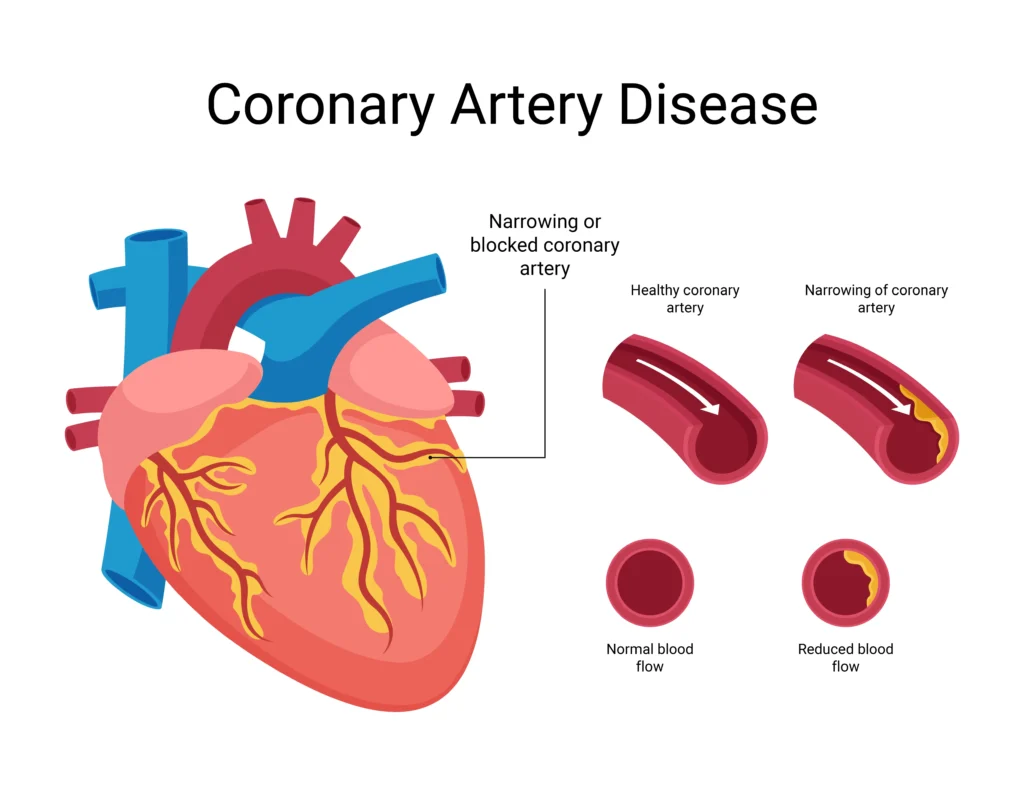
Coronary artery disease (CAD), also known as coronary heart disease, is the most prevalent form of heart disease globally and the leading cause of death in the United States. It occurs when the arteries supplying blood to the heart muscle become narrowed or completely blocked, typically due to the buildup of plaque—a sticky substance composed of fat, cholesterol, calcium, and other materials. This plaque accumulation limits blood flow to the heart, depriving it of the oxygen and nutrients it needs to function properly. Over time, reduced blood flow can lead to chest pain, shortness of breath, or even heart attacks and sudden cardiac arrest.
CAD develops gradually, often without noticeable symptoms in its early stages. That’s why understanding the condition—its causes, warning signs, risk factors, and ways to prevent or manage it—is critical to protecting your heart health and overall well-being. Whether you’re newly learning about CAD, managing existing risk factors, or seeking clinical guidance, this guide offers a complete overview suitable for individuals at all knowledge levels.
Table of Contents
How the Heart Works
The human heart is a vital organ that pumps oxygen-rich blood throughout the body. To perform this task efficiently, the heart itself requires a constant supply of oxygen, which is delivered through the coronary arteries. The two main coronary arteries, the left and right coronary arteries, branch out from the aorta and wrap around the surface of the heart. The left coronary artery primarily supplies the left side of the heart, while the right coronary artery supplies the right side.
When these arteries are clear and healthy, blood flows freely. However, when plaque builds up along the inner walls of these vessels—a process known as atherosclerosis—blood flow becomes restricted. The heart then struggles to receive the oxygen it needs, which can impair its ability to function, especially during physical exertion or emotional stress.
What is Coronary Artery Disease (CAD)?
Coronary artery disease refers to a condition in which the coronary arteries become narrowed or blocked, most commonly due to atherosclerosis. The buildup of plaque makes the arterial walls stiff and narrow, reducing or even completely obstructing blood flow. This blockage can be partial or total, and the consequences range from mild discomfort to life-threatening cardiac events.
Different manifestations of CAD exist depending on the extent of blockage and the presence or absence of symptoms. Some individuals experience stable angina, a predictable pattern of chest pain during physical activity or stress that usually resolves with rest or medication. Others may suffer from unstable angina, which is more unpredictable and could signal an impending heart attack. In more severe cases, a total blockage leads to a myocardial infarction, or heart attack. There’s also a form of CAD known as silent CAD, in which individuals experience no noticeable symptoms despite significant damage to the heart muscle.
| Type | Description |
|---|---|
| Stable Angina | Predictable chest pain during exertion or stress |
| Unstable Angina | Unpredictable and potentially more dangerous chest pain |
| Myocardial Infarction (Heart Attack) | Complete blockage of coronary artery causing tissue death |
| Silent CAD | No symptoms but underlying damage is occurring |
Causes of CAD
The primary cause of CAD is atherosclerosis, which involves the accumulation of plaque along the inner lining of the coronary arteries. This plaque is composed of fat, cholesterol, calcium, and other cellular waste products. As plaque builds up over time, the arteries narrow and become less flexible, restricting blood flow to the heart.
This condition is often exacerbated by several contributing factors. High levels of low-density lipoprotein (LDL) cholesterol—often referred to as “bad” cholesterol—are particularly harmful, as LDL tends to deposit within the arterial walls. On the other hand, low levels of high-density lipoprotein (HDL) cholesterol, or “good” cholesterol, reduce the body’s ability to remove excess cholesterol. Elevated blood pressure can damage the arterial walls, making it easier for plaque to form. Smoking introduces harmful chemicals into the bloodstream that damage blood vessels and contribute to inflammation and plaque buildup.
Diabetes, particularly when poorly managed, increases CAD risk by accelerating atherosclerosis. Obesity and a sedentary lifestyle also play significant roles, as both are associated with poor lipid profiles, high blood pressure, and insulin resistance. Inflammation, whether due to chronic conditions like lupus or external factors such as pollution, may also trigger or worsen the development of CAD.
Common and Subtle Symptoms
Coronary artery disease does not always cause noticeable symptoms, especially in its early stages. When symptoms do occur, they are often the result of reduced blood flow to the heart during exertion or stress. One of the most common symptoms is angina, which is typically described as a pressure, heaviness, tightness, or pain in the chest. This discomfort may radiate to the shoulders, arms, neck, jaw, or back.
Shortness of breath during physical activity or even while at rest can also be a warning sign, especially if it occurs without another obvious cause. Fatigue is another frequent symptom, particularly in women and older adults. It’s not unusual for individuals to report feeling unusually tired even after minimal exertion.
Interestingly, CAD symptoms can present differently across population groups. Women may experience subtler symptoms such as nausea, indigestion-like sensations, or sleep disturbances. People with diabetes may not feel typical chest pain due to nerve damage affecting pain perception, a condition known as silent ischemia.
| Population Group | Unique Symptoms |
|---|---|
| Women | More likely to experience back/jaw pain, nausea |
| Elderly | May only feel fatigue or shortness of breath |
| Diabetics | Often experience “silent” CAD due to nerve damage |
Risk Factors: Who’s Most at Risk?
The likelihood of developing CAD increases significantly when certain risk factors are present. These risk factors can be categorized into modifiable and non-modifiable elements.
Modifiable risk factors include lifestyle and medical conditions that can be addressed through behavioral changes or treatment. For instance, high blood pressure, elevated LDL cholesterol, diabetes, smoking, physical inactivity, and unhealthy eating habits are all factors that, if managed properly, can reduce one’s risk of CAD. Obesity, particularly abdominal obesity, is associated with a higher incidence of heart disease due to its links with insulin resistance and systemic inflammation.
On the other hand, non-modifiable risk factors such as age, sex, and genetic predisposition cannot be changed. Men over the age of 45 and women over 55 have a higher risk of developing CAD, and those with a family history of early heart disease are also more vulnerable. Additional emerging risk factors include sleep apnea, excessive stress, chronic inflammation, and even certain autoimmune diseases.
| Category | Risk Factor Examples |
|---|---|
| Modifiable | High cholesterol, smoking, high blood pressure, poor diet, inactivity, diabetes |
| Non-Modifiable | Age (men >45, women >55), family history, genetics |
| Emerging Risks | Chronic stress, sleep apnea, systemic inflammation |
How CAD is Diagnosed
Diagnosing coronary artery disease involves a comprehensive evaluation that includes a review of medical history, a physical examination, and a variety of diagnostic tests. Physicians often begin with an electrocardiogram (EKG or ECG), which records the electrical signals of the heart and helps identify irregular heart rhythms or past heart attacks.
If CAD is suspected, a stress test may be performed. This involves exercising on a treadmill or taking medication that simulates exercise while heart activity is monitored. Stress tests can reveal problems that only become apparent when the heart is under strain.
An echocardiogram, or ultrasound of the heart, provides real-time images of heart structure and function. For more detailed views, computed tomography (CT) coronary angiography or invasive cardiac catheterization may be used to visualize blockages directly.
| Test | Purpose |
|---|---|
| Electrocardiogram (ECG or EKG) | Detects irregular heart activity |
| Stress test | Monitors heart during physical exertion |
| Echocardiogram | Ultrasound image of heart structure/function |
| CT Coronary Angiography | Non-invasive imaging to view arteries |
| Cardiac Catheterization | Invasive procedure to examine blockage directly |
Complications of Untreated CAD
Left untreated, CAD can result in a cascade of serious and potentially life-threatening complications. The most critical is a myocardial infarction, or heart attack, which occurs when a coronary artery becomes completely blocked, cutting off blood flow to part of the heart muscle. Without oxygen, the heart tissue begins to die.
In addition to heart attacks, CAD can lead to heart failure—a condition in which the heart becomes too weak to pump blood efficiently. Arrhythmias, or abnormal heart rhythms, may also develop, increasing the risk of stroke or sudden cardiac arrest. Furthermore, untreated CAD can contribute to peripheral artery disease, reducing blood flow to the limbs, and increase the risk of ischemic stroke if clots formed in the heart travel to the brain.
Treatment and Management Options
Treatment of CAD aims to restore blood flow, relieve symptoms, and prevent future complications. Most treatment plans begin with lifestyle interventions and medications. Statins are commonly prescribed to lower cholesterol levels, while beta-blockers and ACE inhibitors help manage blood pressure and reduce the heart’s workload. Aspirin or other antiplatelet agents are often used to prevent clot formation. In cases of angina, nitrates may be prescribed to widen blood vessels and relieve chest pain.
When lifestyle changes and medications are not enough, surgical interventions may be required. Angioplasty involves inflating a small balloon inside the narrowed artery to widen it, often followed by placement of a stent to keep the artery open. In more advanced cases, coronary artery bypass grafting (CABG) may be performed to create new pathways for blood to reach the heart muscle.
Lifestyle Changes for Prevention and Recovery
Making lasting lifestyle changes is one of the most effective ways to prevent and manage CAD. Quitting smoking, maintaining a healthy weight, engaging in regular physical activity, and following a heart-healthy diet can significantly reduce risk and improve outcomes. Managing stress through mindfulness, therapy, or relaxation techniques also supports heart health. Reducing alcohol intake and ensuring adequate sleep further contribute to cardiovascular well-being.
Nutrition and CAD
Diet plays a crucial role in both the prevention and treatment of CAD. A balanced eating plan rich in vegetables, fruits, whole grains, lean proteins, and healthy fats can help lower cholesterol and reduce inflammation. The DASH and Mediterranean diets are widely recommended for individuals at risk of or living with CAD.
| Food Group | Eat More | Avoid |
|---|---|---|
| Vegetables & fruits | ✓ | — |
| Whole grains | ✓ | Refined grains |
| Lean proteins | ✓ | Processed meats |
| Healthy fats (olive oil, nuts) | ✓ | Trans fats, fried foods |
| Low-fat dairy | ✓ | Full-fat dairy |
Exercise and Physical Activity Guidelines
Physical activity strengthens the heart muscle and improves circulation. Most health authorities recommend at least 150 minutes of moderate-intensity aerobic exercise each week, such as brisk walking, swimming, or cycling. Strength training exercises should also be included at least two days per week. For older adults or those recovering from a cardiac event, balance and flexibility exercises like tai chi or gentle yoga can be beneficial.
Mental Health and Stress in CAD
Stress and poor mental health can exacerbate CAD. Chronic stress triggers inflammation and elevates blood pressure and heart rate. Depression is also linked to poorer heart health outcomes. Managing stress effectively is crucial. Cognitive behavioral therapy, meditation, social support, and getting adequate sleep all contribute to emotional resilience and cardiovascular health.
References
Centers for Disease Control and Prevention. (2023). Coronary Artery Disease (CAD). https://www.cdc.gov/heart-disease/about/coronary-artery-disease.html
American Heart Association. (2023). Coronary Artery Disease – Coronary Heart Disease. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/coronary-artery-disease
National Heart, Lung, and Blood Institute. (2023). What Is Coronary Heart Disease? https://www.nhlbi.nih.gov/health/coronary-heart-disease
Mayo Clinic. (2024). Coronary artery disease. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease




0 Comments