Coronary artery disease (CAD), also referred to as ischemic heart disease, remains the leading cause of death worldwide. According to the World Health Organization (2024), an estimated 17.9 million lives are lost to cardiovascular diseases each year, with CAD accounting for over 40% of these fatalities. Often developing silently over decades, CAD culminates in life-altering events such as heart attacks, heart failure, and sudden cardiac death. The insidious nature of the disease—where symptoms may not appear until critical damage has occurred—underscores the necessity for early detection and proactive management.
This article aims to provide a comprehensive overview of coronary artery disease, examining its causes, symptoms, diagnostic tools, treatment options, and preventive strategies. Grounded in the latest clinical research, it emphasizes the role of early intervention and evidence-based care in improving patient outcomes and reducing the global burden of cardiovascular disease.
Table of Contents
Understanding Coronary Artery Disease: What Is It?
Coronary artery disease is a condition characterized by the narrowing or blockage of coronary arteries due to atherosclerosis—the buildup of fatty deposits (plaque) inside the arterial walls. Over time, this buildup restricts blood flow to the heart muscle, depriving it of oxygen and nutrients. In some cases, a plaque may rupture, triggering the formation of a blood clot that can completely obstruct the artery, resulting in a myocardial infarction, or heart attack.
The Atherosclerotic Process
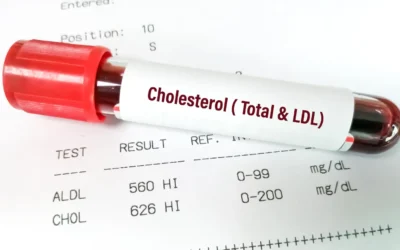
Atherosclerosis begins when low-density lipoprotein (LDL) cholesterol penetrates the inner lining of the arterial wall. Oxidized LDL triggers an inflammatory response, leading to the recruitment of immune cells, smooth muscle proliferation, and fibrous cap formation. The resulting plaque may be stable or vulnerable—prone to rupture and thrombosis.
Causes and Risk Factors: What Drives CAD?
While atherosclerosis is the primary pathological mechanism, the development of CAD is influenced by a constellation of modifiable and non-modifiable risk factors. Understanding these can guide both prevention and treatment strategies.
| Risk Factor | Description |
|---|---|
| High LDL Cholesterol | Promotes plaque formation in coronary arteries |
| Hypertension | Damages arterial walls, facilitating plaque accumulation |
| Smoking | Contributes to endothelial dysfunction and promotes clot formation |
| Type 2 Diabetes | Increases inflammation and lipid abnormalities |
| Obesity and Physical Inactivity | Associated with insulin resistance, hypertension, and dyslipidemia |
| Family History of CAD | Genetic predisposition elevates lifetime risk |
| Age and Sex | Risk increases with age; men typically at higher risk before age 65 |
| Chronic Stress | Elevates blood pressure and promotes unhealthy coping behaviors |
Even with a strong genetic predisposition, the interplay between lifestyle and environmental exposures significantly determines disease onset and progression.
Recognizing the Symptoms: How CAD Manifests
Coronary artery disease can remain asymptomatic for years until it presents as angina or a heart attack. Symptom recognition is crucial for timely intervention.
Common Symptoms
- Angina Pectoris: Chest pain or discomfort, typically triggered by exertion or stress and relieved by rest or nitroglycerin.
- Shortness of Breath: May occur during physical activity or even at rest, indicating heart failure or extensive ischemia.
- Fatigue: A frequent but nonspecific symptom, especially among women.
- Heart Attack (Myocardial Infarction): Severe chest pain, often accompanied by sweating, nausea, lightheadedness, and pain radiating to the left arm or jaw.
It is noteworthy that symptoms often differ by sex. Women may experience atypical presentations such as indigestion, back pain, or extreme fatigue, making diagnosis more challenging.
Diagnosing Coronary Artery Disease: Tools and Techniques
Early and accurate diagnosis of CAD is essential for preventing acute events and initiating appropriate therapy. Modern diagnostics combine clinical evaluation with advanced imaging and stress testing.
Common Diagnostic Tools
| Test | Purpose |
|---|---|
| Electrocardiogram (ECG) | Detects arrhythmias, prior infarctions, and ischemic changes |
| Echocardiogram | Assesses heart structure and function |
| Exercise Stress Test | Evaluates heart function during exertion |
| Coronary Calcium Scoring (CT) | Quantifies calcified plaque burden |
| Coronary CT Angiography (CTA) | Non-invasive imaging of coronary artery blockages |
| Cardiac Catheterization | Gold standard for detecting and treating obstructive CAD |
| Cardiac MRI | Offers detailed structural and functional cardiac information |
Recent innovations, such as quantitative perfusion cardiac magnetic resonance imaging (qCMR) and FFR-CT (fractional flow reserve computed tomography), provide improved accuracy in identifying functionally significant lesions.
Treatment Strategies: Managing CAD Effectively
The management of coronary artery disease is tailored to the severity of the disease, symptom burden, and the presence of comorbid conditions. Treatment generally falls into three major categories: lifestyle modification, pharmacologic therapy, and revascularization procedures.
Lifestyle Changes: Foundation of All Care
Clinical guidelines universally endorse lifestyle interventions as first-line therapy for both prevention and management of CAD.
- Heart-Healthy Diet: Emphasizes fruits, vegetables, whole grains, lean proteins, and limits saturated fats and sodium.
- Regular Physical Activity: At least 150 minutes per week of moderate aerobic activity is recommended.
- Smoking Cessation: Quitting smoking dramatically reduces CAD risk within a few years.
- Weight Management: Sustaining a healthy BMI reduces cardiac workload and improves metabolic parameters.
- Stress Reduction: Techniques like mindfulness, cognitive behavioral therapy, and yoga have shown benefits in reducing cardiac events.
Medications: Controlling Risk and Symptoms
| Medication Class | Function |
|---|---|
| Statins | Lower LDL cholesterol and stabilize plaque |
| Antiplatelet Agents (e.g., aspirin) | Prevent clot formation |
| Beta-Blockers | Reduce heart rate and myocardial oxygen demand |
| ACE Inhibitors / ARBs | Lower blood pressure, reduce cardiac remodeling |
| Nitrates | Relieve chest pain by dilating blood vessels |
| SGLT2 Inhibitors / GLP-1 RAs | Emerging options in diabetic patients with cardiovascular disease |
Evidence from the ISCHEMIA trial and other studies suggests that optimal medical therapy (OMT) alone can be as effective as revascularization in certain patients with stable CAD, highlighting the need for individualized care plans.
Revascularization: When Medication Isn’t Enough
In more advanced cases or when medical therapy fails to control symptoms, procedural intervention may be warranted.
- Percutaneous Coronary Intervention (PCI): A minimally invasive procedure involving balloon angioplasty and stent placement.
- Coronary Artery Bypass Graft Surgery (CABG): Involves rerouting blood flow using grafts from other vessels.
Revascularization has proven survival benefits in patients with left main coronary disease, multi-vessel disease with diabetes, or reduced ejection fraction.
Preventing CAD: A Lifespan Approach
The most effective strategy against CAD is prevention. Targeting risk factors through public health efforts and personal choices can significantly reduce the burden of disease.
Key Preventive Measures
- Regular Health Screenings: Early identification of hypertension, hyperlipidemia, and diabetes.
- Routine Physical Activity: Enhances endothelial function and insulin sensitivity.
- Dietary Management: Mediterranean-style diets have been shown to reduce cardiovascular events.
- Alcohol Moderation: Excessive drinking is linked to hypertension and atrial fibrillation.
- Vaccinations: Influenza and COVID-19 vaccines reduce cardiac complications in high-risk individuals.
A growing emphasis on primordial prevention—preventing the emergence of risk factors altogether, particularly in children and adolescents—may be the next frontier in cardiovascular care.
Prognosis and Life Expectancy: What Patients Should Know
With prompt treatment and long-term management, many individuals with CAD can lead active lives. Prognosis depends on the extent of coronary involvement, ejection fraction, lifestyle changes, and adherence to medical therapy. Studies show that patients who maintain rigorous secondary prevention regimens—including smoking cessation, statin adherence, and physical activity—can experience a 30–50% reduction in future cardiac events.
Nonetheless, untreated or poorly managed CAD significantly increases the risk of heart failure, arrhythmias, and sudden cardiac death.
Conclusion: Confronting CAD with Knowledge and Action
Coronary artery disease remains a leading cause of global morbidity and mortality, but it is far from inevitable. Through a comprehensive understanding of its causes, symptoms, and risk factors—paired with cutting-edge diagnostic tools and evidence-based interventions—individuals and clinicians alike can work to prevent or manage this life-threatening condition.
The keys to improving outcomes lie in early detection, consistent lifestyle changes, and personalized medical therapy. As the landscape of cardiovascular care evolves, integrating the latest research into practice will ensure that more lives are not only saved but also enriched with quality and longevity.
References
- World Health Organization. (2024). Cardiovascular diseases (CVDs). Retrieved from https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- American Heart Association. (2023). Heart Disease and Stroke Statistics – 2023 Update. Retrieved from https://www.heart.org
- UPMC. (2024). Coronary Artery Disease. Retrieved from https://www.upmc.com/services/heart-vascular/conditions/coronary-artery-disease
- ISCHEMIA Research Group. (2020). Initial Invasive or Conservative Strategy for Stable Coronary Disease. New England Journal of Medicine, 382(15), 1395-1407.
- Mayo Clinic. (2024). Coronary Artery Disease Diagnosis and Treatment. Retrieved from https://www.mayoclinic.org
- National Institutes of Health. (2024). Understanding Coronary Heart Disease. Retrieved from https://www.nhlbi.nih.gov
- UVA Health. (2024). Technique Improves Coronary Artery Disease Diagnosis. Retrieved from https://newsroom.uvahealth.com
- Circulation. (2023). Guideline for the Management of Patients with Chronic Coronary Disease. https://www.ahajournals.org/doi/10.1161/CIR.0000000000001168




0 Comments